46
Vol. 66, No. 3 2015
Northeast Florida Medicine
Endovascular Neurosurgery
Technique
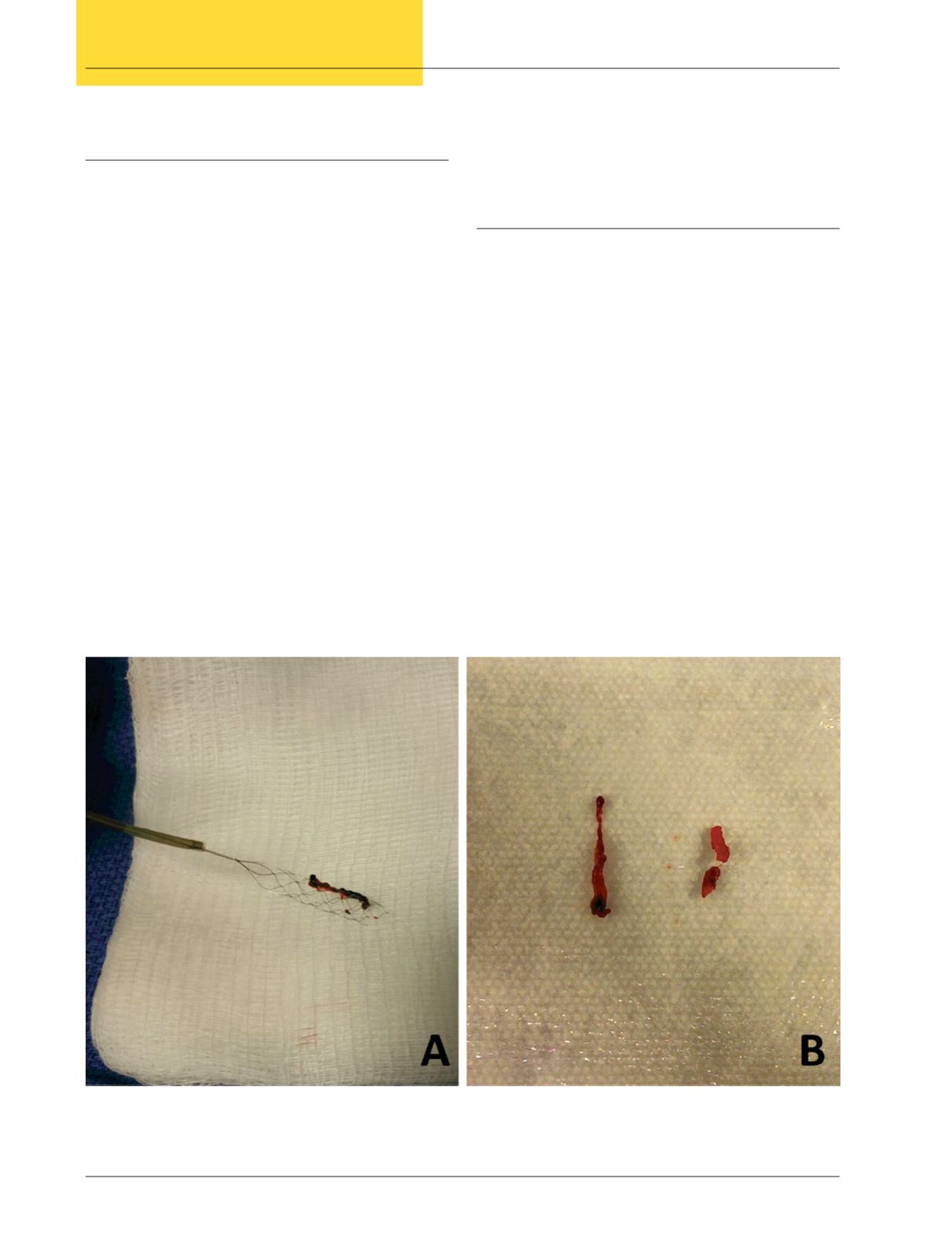
Although it is beyond the scope of this article to discuss
the merits of one endovascular technique over another, me-
chanical thrombectomy using stentrievers (self-expanding
tube-like devices composed of a metallic mesh) has amassed
considerable support and acceptance after the publication
of the aforementioned clinical trials.
Patients considered appropriate candidates for acute
stroke intervention are placed supine on the angiography
table. Conscious sedation is favored over general anesthesia
to prevent hypotension and avoid delays in reperfusion. A
femoral approach is most frequently used and a guiding
catheter is positioned in the cervical vessel at the level of the
skull base. Using contrast injections and roadmap guidance,
a microcatheter is gently advanced through the occluded
vessel over a distance likely to be distal to the thrombus/
embolus. At this point, the stentriever or another device is
deployed. As the device expands, it pushes the clot against
the blood vessel wall causing an immediate restoration of
flow and perfusion to the ischemic brain while at same time
embedding the clot within the struts of the device (Figure
3). As the catheter and device are carefully pulled out, suc-
tion is performed to prevent dislodgment of small pieces of
the clot and distal embolization. At the conclusion of the
procedure, the patient is transferred for close monitoring
in the neurointensive care unit.
Discussion and Conclusion
In resounding fashion these recent clinical trials have
shownunprecedented outcomes with endovascular treatment
of ischemic stroke, driven by state of the art technology,
optimized patient selection and reduced door-to-groin
puncture times. The absolute benefit of endovascular treat-
ment compared to IV t-PA alone measured by functional
independence at 90 days (mRS score ≤ 2) ranged from 13.5
to 31 percentage points. This can be translated into a num-
ber needed to treat as low as 3 patients and no more than
7 patients in order to obtain clinical benefit. These figures
are impressive considering that 17 patients with STEMI are
needed in order to prevent one myocardial infarction/stroke
or deathwithpercutaneous coronary intervention.The future
of stroke therapy now requires adapting the infrastructure
to include endovascular angiosuites and rapid protocols to
identify salvageable brain tissue. There are now protocols
that have optimized rapid response strategies in patients with
suspected large vessel occlusion. For instance, patients with
high index of suspicion for stroke are quickly scanned to
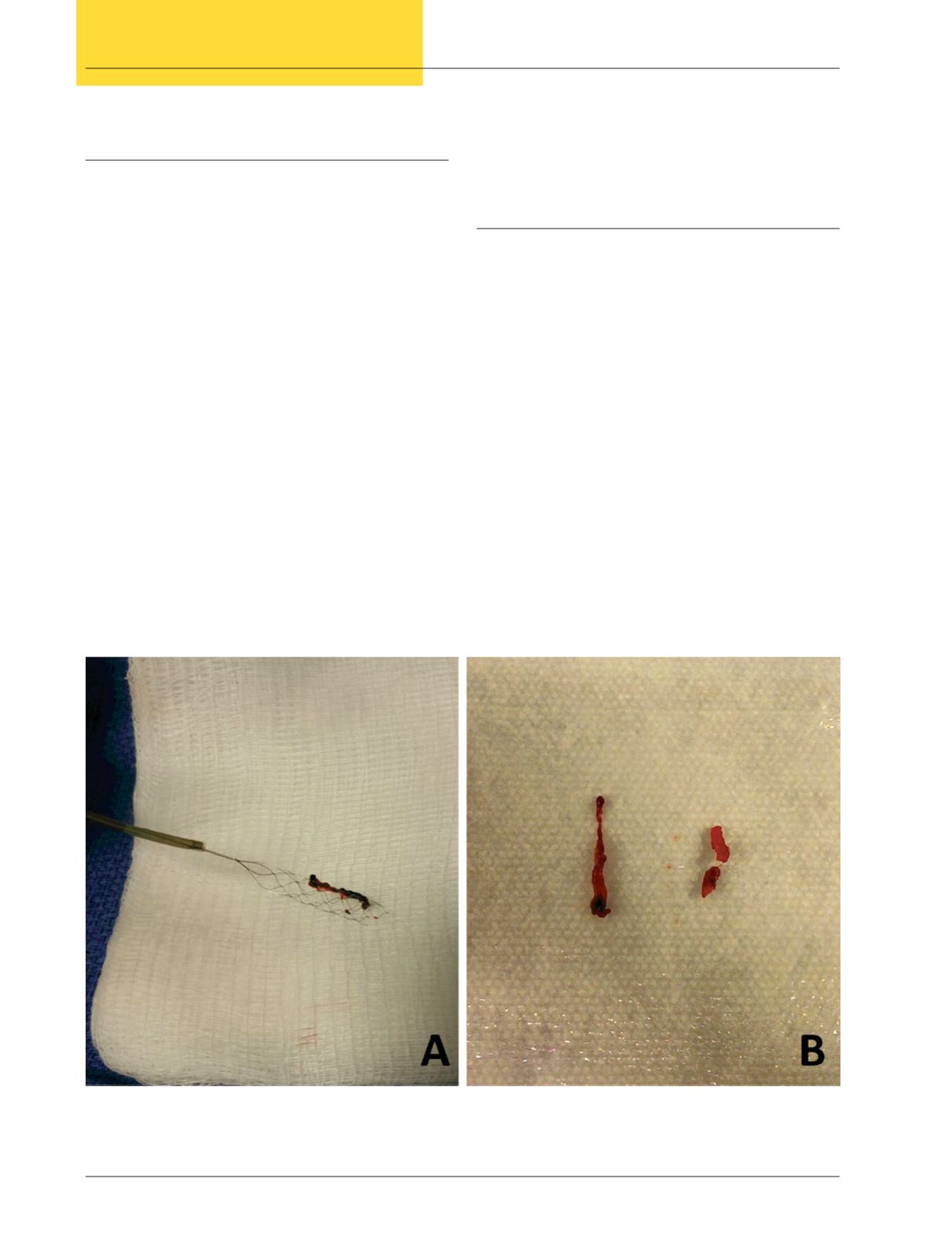
Figure 3.
Photographs depicting a clot removed with a stentriever from a patient with complete occlusion of the middle
cerebral artery. Panel A shows the material attached to the mesh of the device immediately after removal. Panel B shows in a
magnified view the macroscopic characteristics of the clot.