58
Vol. 66, No. 1 2015
Northeast Florida Medicine
Otolaryngology
of the genetic causes of hearing loss, the search for hearing
restoration through molecular, gene and stem cell thera-
pies is rapidly moving forward. Successful manipulation
of the genes within the cochlea of laboratory animals has
led to human trials.
4
The transfer of genetic information
into the human genome for patients affected with Usher’s
Syndrome 1B is one such example. This genetic transfer
corrects for the abnormal myosin, which occurs in the ears
and eyes (MYO7A) of these patients. Several animal studies
are currently underway looking at introduction of genetic
information to correct for DFNB1, which codes for a gap
junction protein representing the most common cause of
autosomal recessive genetic deafness. Human clinical trials
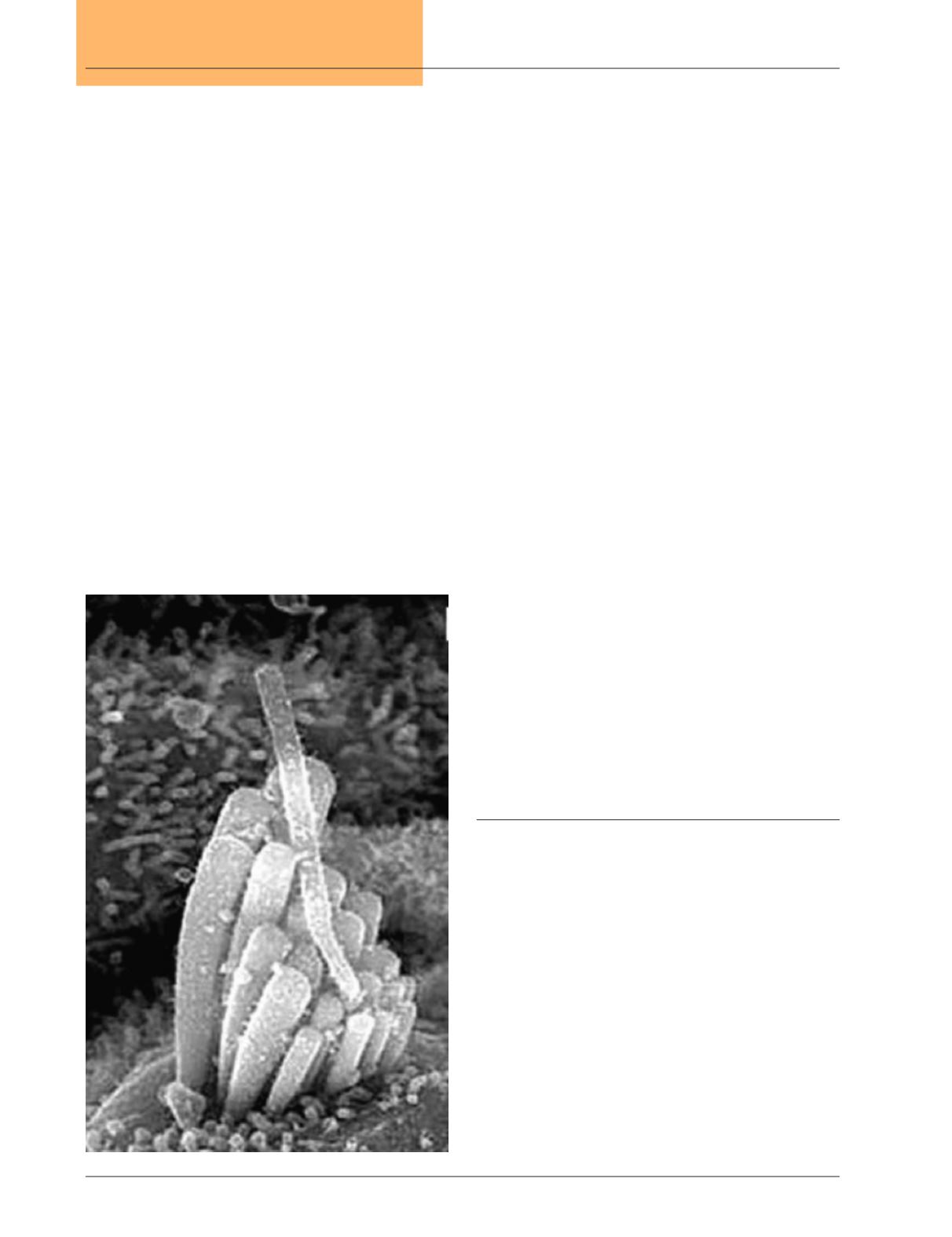
using Atoh1, a basic, helix-loop-helix transcription factor
have recently been approved for patients with acquired
deafness to allow for hair cell regeneration. (Figure 3) Oth-
er trials are underway looking at the use of brain derived
neurotrophic factor (BDNF) to help preserve/regenerate
spiral ganglion cells.
24
BDNF also is being incorporated in
cochlear implant electrode arrays to help direct dendritic
growth towards the electrodes.
The use of stem cells for regeneration of hair cells is also
showing great hope for patients with genetic and acquired
hearing loss. Several studies have demonstrated the ability
to grow hair cells in vivo using step-wise differentiation
from inner ear progenitor cells.
25
Problems persist in the
orientation of these stem cells, as well as the ingrowth of
dendritic connections fromthe spiral ganglion. Nevertheless,
it represents a tremendous step forward to help our patients
with various forms of hearing loss. Efforts to generate spiral
ganglion auditory neurons from stem cells are also under-
way. These efforts may help patients undergoing cochlear
implantationwho have a severe loss of ganglion cells limiting
the effectiveness of the cochlear implant.
Endogenous signaling mechanisms allow the pluripotent
supporting cells of the cochlea to develop into functional
hair cells in birds and lower vertebrates. Better understand-
ing of these signaling mechanisms has led to the use of
pharmacologic agents such as a gamma-secretase inhibitor
to block notch signaling and thereby reduce lateral inhi-
bition between hair cells and supporting cells. The use of
an antisense oligonucleotide (ASO) in a mouse model of
Usher Syndrome 1C has also shown promise in allowing
growth of functional hair cells. While effective only at a very
early developmental stage, this therapy may prove to be an
alternative to inserting genetic material into the cochlea.
26
Conclusion
As the complexities of hearing are better understood, new
strategies for helping our patients with deafness will undoubt-
edly unfold.These strategies will need to target multiple areas
of the inner ear and central nervous system. The timing of
various treatment options within the developmental process
from the otic placode stage to the fully developed cochlea
will also need to be considered. The miracle of hearing with
connection to others represents one of our most important
sensory systems with incredible opportunities to ease the
burden of those suffering fromhearing loss. Sound strategies
to help our patients are available now with more exciting
treatment options on the horizon.
Figure 3.
A hair-like cell generated via a gene-therapy
strategy and viral-mediated delivery of the
transcription factor Atoh1 into the inner ear of a
deaf guinea pig. (Reprinted from Kawamoto et al.,
J Neurosci 23, 4395-4400 (2003))