Northeast Florida Medicine
Vol. 66, No. 2 2015
21
Pediatric Oncology
Introduction
One of the three main treatments of tumors, radiation
therapy is a powerful tool alongside surgery and chemother-
apy. The target of the radiation beam is primarily the DNA
and other intracellular components of tumors. As tumor cells
develop, their internal repair mechanisms are compromised
because of rapid proliferation compared to normal cells. This
dysfunction in tumor cell repair results in greater destruction
of tumor cells, compared to normal cells from the radiation
beam. When a tumor is treated with a protracted course of
fractionated radiotherapy, which delivers a relatively small
amount of radiation daily, normal cells along the radiation
beam’s path have time to repair any DNA damage between
treatment administrations. In contrast, tumor cells cannot
perform this repair with the same efficiency because of their
mutated state. This differential in damage repair is one of the
fundamentals of radiobiology.
It is estimated that 4,000 children and adolescents were
diagnosed with central nervous system (CNS) tumors in
2014 in the United States.
1
Most of these tumors are sporadic,
developing in those without a family history or other risk
factors. Even very young children can be affected and their
risk of side effects is even higher than their older pediatric
counterparts. While cure is a primary goal in the treatment of
these tumors, both efficacy and toxicity must be considered.
Particularly in children withmany years of life ahead of them,
quality of life and preservation of function are vital.
To this end, tumor targeting and control of the radiation
dose distribution have undergone significant improvements
over the past several decades. Computed tomography (CT)-
based planning is standard-of-care in theUnited States, which
allows for the individualizationof eachradiation treatment plan
for each patient’s anatomy and tumor extent. Other imaging
modalities, such as magnetic resonance imaging (MRI), are
routinely fused to enhance target delineation. When deliv-
ering radiation, linear accelerators are the most commonly
used treatment delivery systems in the United States.
2
They
provide a range of low to high photon energies to reach both
superficial anddeep tumors. Immobilization, patient or tumor
motion, and target accuracy must be rigorously assessed for
each patient to reduce the chance of a marginal miss. Daily
image guidance is often employed to ensure accuracy and
precision. Advances in treatment delivery techniques, such
as intensity-modulated radiation therapy (IMRT), have
resulted in the ability to conform the high dose to the target
The Curative Role of Radiation in
Common Pediatric Brain Tumors
By Julie A. Bradley, MD, Ronny Rotondo, MD, Daniel Indelicato, MD
Abstract:
Although rare, pediatric brain tumors affect hundreds of
children and families every year. Radiation therapy is employed in the
treatment of many of these tumors. For tumors such as ependymoma
and medulloblastoma, radiation therapy decreases the likelihood of a
recurrence following surgery. For other tumors, like craniopharyngio-
mas, radiation therapy is often used as definitive treatment, offering
higher control rates and fewer toxicities than surgical resection
alone. Surgery remains the mainstay of treatment for most low-grade
gliomas. Radiation therapy can be used as definitive treatment for
unresectable tumors, adjuvant treatment for recurrent tumors, or
salvage treatment for tumors that have progressed after surgery and
chemotherapy. Like surgery and chemotherapy, radiation therapy
carries a risk of long-term side effects that require lifelong monitoring.
Advances in radiation treatment technology are being utilized to
diminish these potential late toxicities and improve the therapeutic
ratio of radiotherapy.
Address correspondence to:
Daniel J. Indelicato, MD
University of Florida Proton Therapy Institute
2015 North Jefferson Street
Jacksonville, FL 32206
Telephone: (904) 588-1800; Fax: (904) 588-1300
Email:
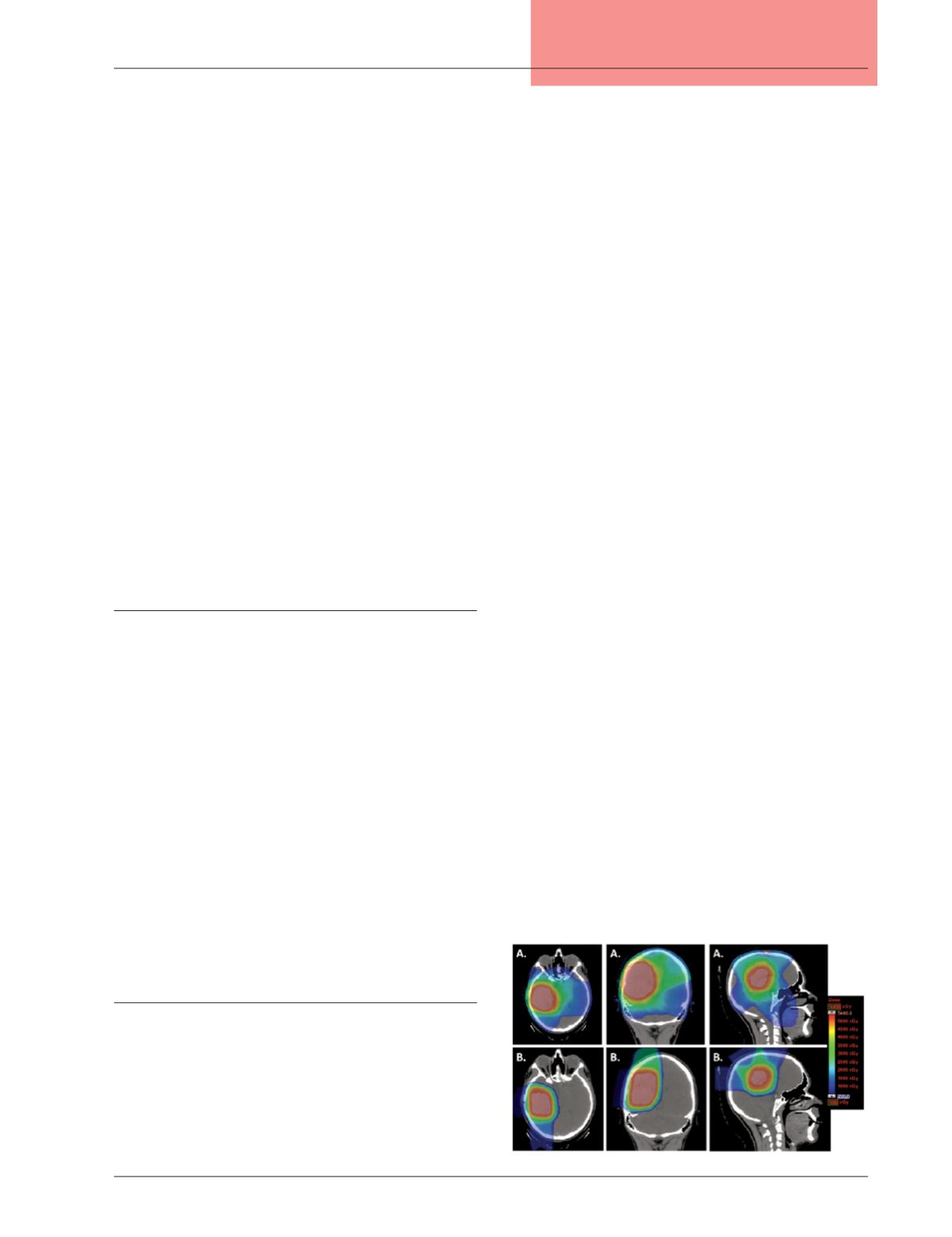
Figure 1:
Dose distribution for a right temperoparietal low-
grade glioma treated with (A) intensity-modulated
radiation therapy compared to (B) proton therapy.