Northeast Florida Medicine
Vol. 66, No. 2 2015
23
Pediatric Oncology
For patients younger than 3 years old, toxicity from exten-
sive radiotherapy in such a sensitive population is of great
concern. Multiple studies have evaluated eliminating radio-
therapy in this population of medulloblastoma patients, or
delivering chemotherapy before radiotherapy to allow more
time for normal tissue development. Some data suggest out-
comes are comparable for young children with GTR treated
with adjuvant chemotherapy alone.
13,14
Nevertheless, most
oncologists favor the latter approach and deliver CSI after
one to two years of chemotherapy. Duffner et al reported no
difference in outcomes when chemotherapy was administered
after surgery and radiation therapy was delayed in young chil-
dren with M0 disease and GTR.
15
Hartsell et al,
16
however,
found an increasing risk of disease progression throughout
the craniospinal axis corresponding to a longer duration of
chemotherapy. The actuarial failure rate in the children ≤ 3
years old was approximately 23 percent, and of all patients
who progressed on chemotherapy, 50 percent were successfully
salvaged with CSI.
TheChildren’sOncologyGroup currently has openprotocols
to de-intensify therapy for children with low-risk medulloblas-
toma by reducing the CSI dose to 18 Gy (ACNS 0331), and
intensifing therapy for those with high-risk disease through
the addition of chemotherapy agents, including concurrent
carboplatin and isotretinoin maintenance therapy (ACNS
0332).
17
New risk stratification based on molecular subtyping
offers an opportunity for further therapeutic refinement. This
new approach stems from recent data focusing on the genetic
heterogeneity of medulloblastomas, establishing four primary
subtypes based on differences in transcriptome (WNT, SHH,
Group 3, Group 4).
18
The subtypes also vary by predilection
for, and site of, recurrence. Investigations to tailor therapy
according to subtype are in development, with decreased or
increased intensity of treatment and location to which that
treatment is focused.
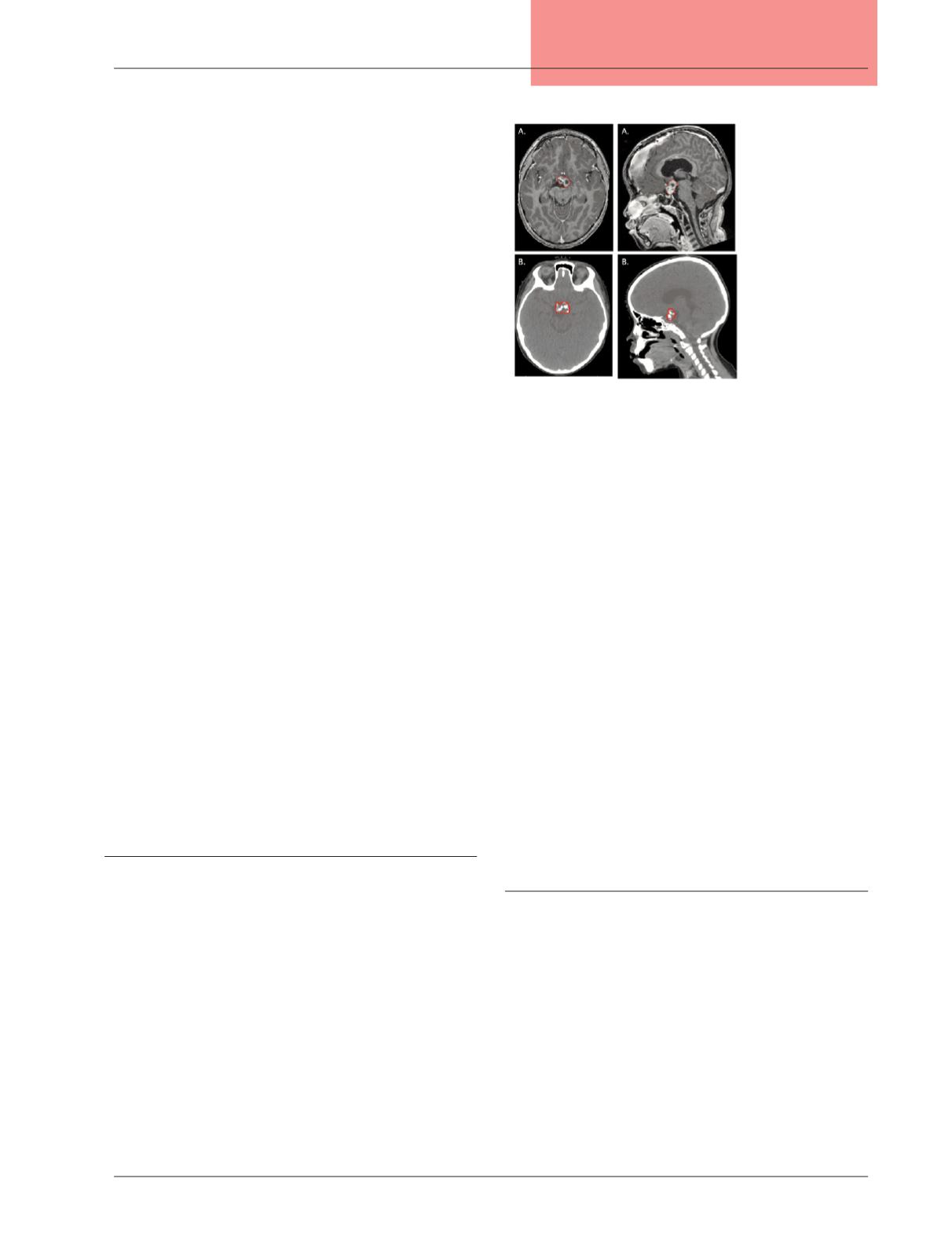
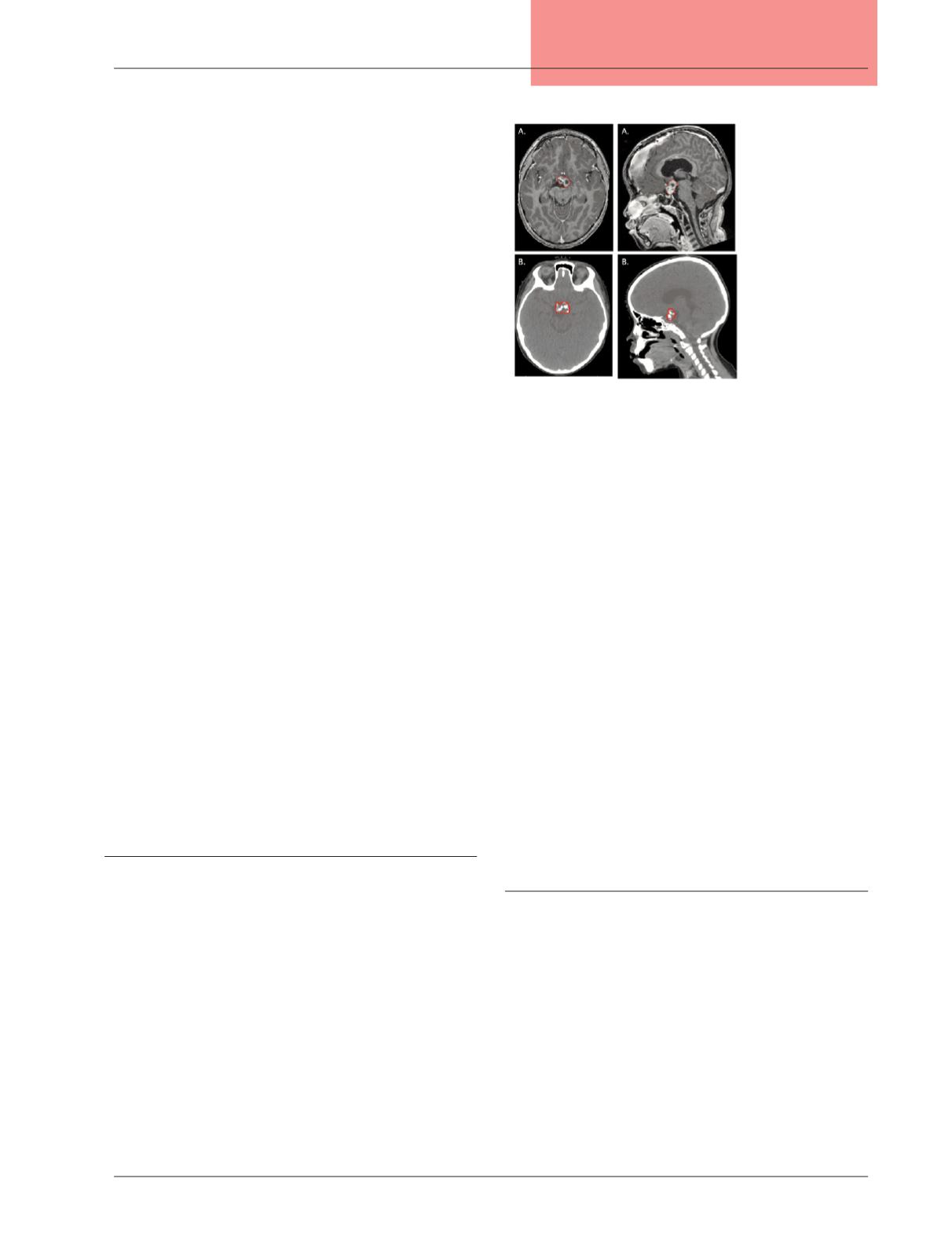
Craniopharyngioma
Craniopharyngiomas are benign tumors that develop in
the suprasellar region, most commonly diagnosed in children
ages 5 to 14. They comprise five percent of pediatric brain
tumors.
8
With this tumor, overall outcomes are not driven by
the extent of surgical resection. Diagnosis can be made from
the characteristic radiographic appearance of solid and cystic
components with calcification if biopsy carries a high risk of
morbidity (Figure 2). Any aggressive surgery can result in
increased toxicity, most frequently diabetes insipidus, without
any benefit in tumor control.
19,20
Therefore, a maximal safe
resection is the surgical goal. In some cases, if the risks of
surgery are estimated to be high, radiotherapy can be used
definitively as the sole treatment modality.
Winkfield et al reported on 79 pediatric patients with
craniopharyngioma treated from 1976 to 2003.
21
43 patients
were treated with limited surgical intervention (one with
GTR, 24 with subtotal resection, and 18 with cyst aspira-
tion) and adjuvant radiotherapy, and 36 with surgery alone.
Radiation therapy was delivered using a variety of photon
techniques, including fractionated stereotactic radiotherapy,
coronal arc therapy, 3-dimensional conformal radiotherapy,
and intensity-modulated radiation therapy. For the entire
cohort, the local control rate was 74 percent at five years and
69 percent at 10 years. The 10-year local control rate was
higher at 84 percent in the patients treated with combined
surgery and radiotherapy.
Radiation therapy is most often delivered with an ex-
ternal beam to a dose of 54 Gy. The cystic components
of the tumor can swell during the course of radiation. If
the tumor is not monitored, an increase in cyst dimen-
sions could push part of the tumor out of the high-dose
radiation field, risking a decline in treatment efficacy.
22
Therefore, the tumor is monitored with weekly MRI. If
the cyst approaches the edge of the high-dose region, the
treatment must be replanned to open the radiation field
in that area. Chemotherapy has not shown benefit in the
treatment of craniopharyngioma.
23
Low-grade glioma
Multiple histologies are classified under the category of
low-grade glioma, including astrocytoma, oligodendro-
glioma, and mixed oligoastrocytoma. All are classified as
World Health Organization grade 1 or grade 2. Low-grade
gliomas are the most common CNS tumor in children.
The age at peak incidence can vary with histology. If the
tumor is resectable, surgery is usually the primary treatment
modality. Following GTR, adjuvant therapy is typically not
necessary unless the surgery is for recurrent disease. Some
low-grade gliomas develop in eloquent areas of the brain and
surgical resection carries a high risk of morbidity. Treatment
options then include chemotherapy, often with vincristine
and carboplatin, or radiation therapy.
Figure 2:
Radiographic image
of craniopharyngioma
on (A) magnetic
resonance imaging
(note the cystic
components) and
(B) computed
tomography (note
the calcifications).