24
Vol. 66, No. 2 2015
Northeast Florida Medicine
Pediatric Oncology
A radiation dose in the range of 50.4 Gy to 54 Gy is required
to treat low-grade gliomas. Merchant et al4 reported on 78
pediatric patients treated with radiotherapy for low-grade
glioma. No patient underwent a GTR prior to radiotherapy
(no biopsy, n=13; biopsy, n=30; and subtotal resection; n=
35). The five-year event-free survival rate was 87.4 percent.
The 10-year event-free survival rate was 74.3 percent and
the 10-year overall survival rate was 95.9 percent. The five-
year progression-free survival rate with chemotherapy alone
ranges from 35 percent to 61percent.
24-26
A recent report
from the Surveillance, Epidemiology, and End Results
(SEER) database of 4,040 children with low-grade glioma
has demonstrated a 20-year overall survival rate of 87 per-
cent, with a 20-year cumulative incidence of death owing to
glioma of 12 percent.
27
In this study, radiation therapy was
a negative prognostic factor for survival. The SEER database
does not provide further details to explore the etiology of the
negative association with radiation, but it most likely arises
from selection bias. Furthermore, this study highlights the
possible lifelong morbidity and treatment-related mortality
in these highly curable brain tumors. With all interventions,
minimizing side effects is a top priority.
Radiotherapy toxicities
There is a potential for both acute and late side effects
from radiation therapy for pediatric brain tumors. The side
effect profile differs depending on the radiation dose, use
of chemotherapy, extent of baseline symptoms, and tumor
location (e.g., in an eloquent region of the brain or near
the periphery). Acute side effects can include fatigue and
symptoms of increased intracranial pressure (ICP) such as
headaches, nausea, and emesis. Dexamethasone can be used
to manage signs or symptoms of increased ICP. Patients with
tumors near the periphery of the brain parenchyma can
experience erythema and desquamation of the skin, along
with alopecia. These symptoms are typically temporary and
manageable. Late effects are of greater concern, especially in
young patients expected to live for many decades. In a study
of 29 pediatric patients treated with photon radiation for
low-grade glioma, with a median follow-up of 17.8 years,
65 percent developed ≥ grade 3 late toxicity.
28
At 10 or
more years after completing radiation therapy, 30 percent
developed a significant cognitive disability and 14 percent
succumbed to treatment-related complications. Neurocogni-
tive dysfunction, including difficulty with processing speed,
memory, and concentration, as well as a decline in IQ, can
irreversibly develop over time.
29-31
There is a small risk of brain
or brainstem necrosis, which could be life-threatening.
4,32-34
Decline in vision, hearing, and neuroendocrine function
can gradually develop and lead to lasting deficits. There is a
risk of radiation-induced vasculopathy, precipitating a stroke.
In a review of children with medulloblastoma treated with
conventional radiotherapy with a median follow-up of 15.4
years, Christopherson et al report 39 percent with ≥ grade 2
hearing loss, 10 percent with cerebrovascular accident, and
24 percent with endocrine abnormalities.
35
Cosmetic sequela,
such as permanent alopecia or facial bone asymmetry, can
also affect these young children. Second tumors or malig-
nancies can also develop in the radiation field decades after
radiation therapy.
36, 37
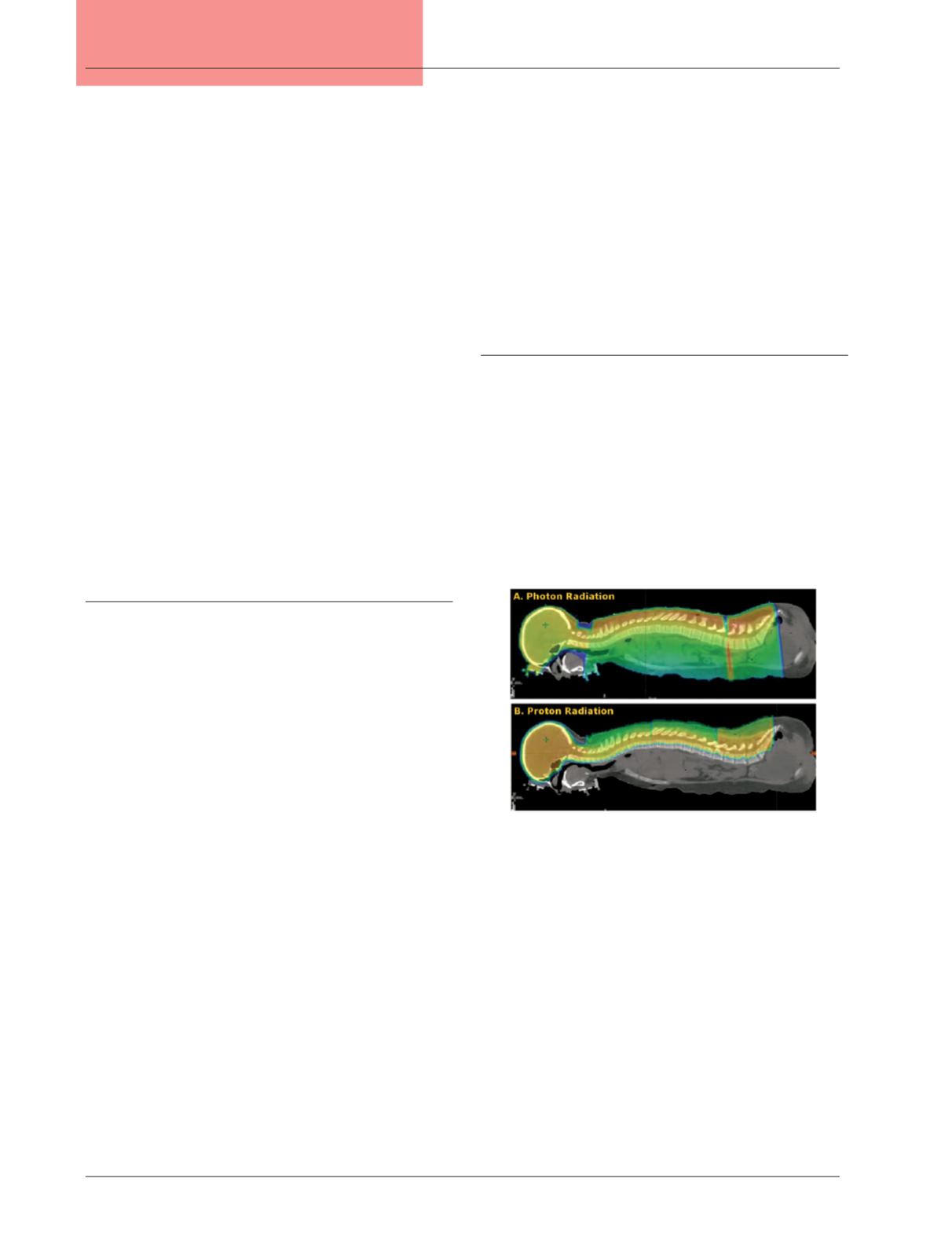
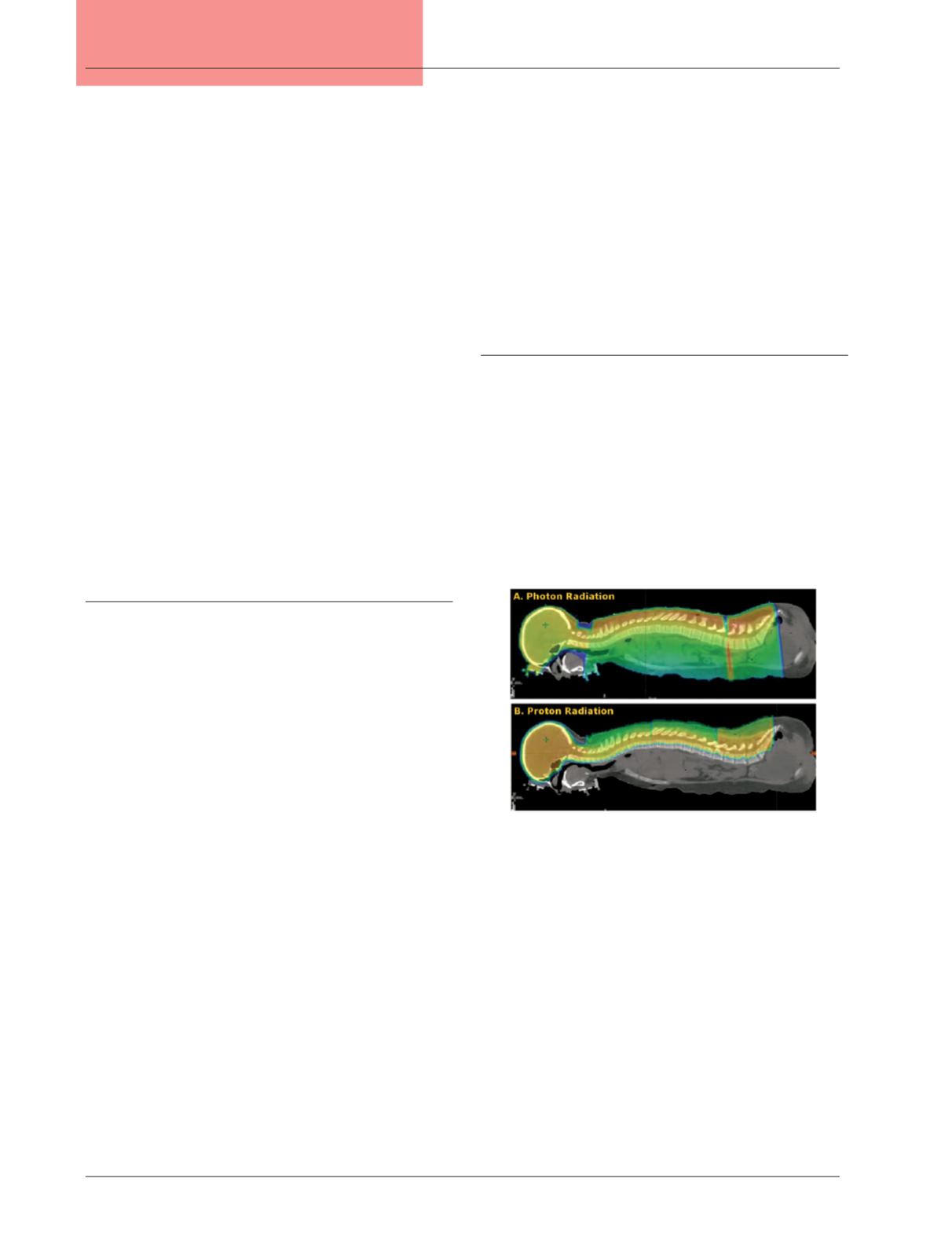
Proton therapy
Proton therapy is a promising approach to mitigating acute
and late toxicities from radiation therapy by eliminating excess
low to moderate radiation dose, reducing the dose to critical
structures, and decreasing the integral body dose (Figure 3).
Proton therapy has been available in the United States for
more than 50 years in a few locations, but has become more
widespread over the past decade. Despite the limited long-term
follow-up and patient population available for studies in proton
therapy, dosimetric investigations and early clinical results have
supported its efficacy and exhibited reductions in toxicity.
In 2013, 722 pediatric patients were treated with proton
therapy at 11 centers in the United States.
38
Overall, 57
percent were less than 10-years-old and nearly half required
daily anesthesia for radiotherapy delivery. The three types of
tumorsmost commonly treated consistedofmedulloblastoma,
ependymoma, and low-grade glioma.Most of the patientswere
treated at three academic institutions, with the University of
Florida Proton Therapy Institute in Jacksonville treating the
most in the country, as it has done consistently for four years.
Figure 3:
Comparison of dose distribution for treatment of
medulloblastoma with craniospinal irradiation using
either (A) photons or (B) protons. Note the elimination
of exit dose through all of the structures anterior to the
vertebral bodies with proton radiation.