Northeast Florida Medicine
Vol. 66, No. 3 2015
35
Endovascular Neurosurgery
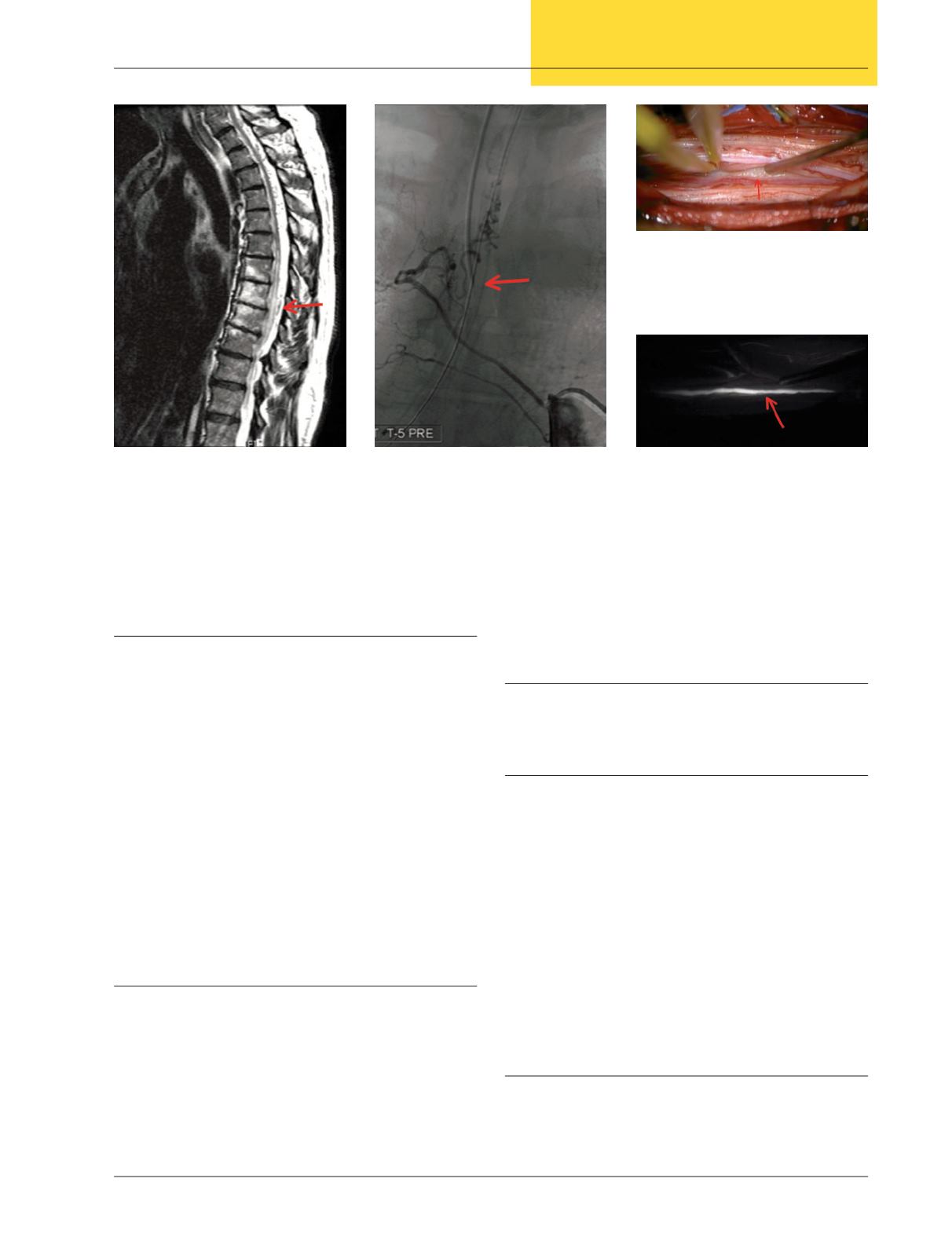
point though spinal angiography remains the gold standard
(Figure 1).
12,13
Selective spinal angiography (SSA)
Even with advances in MRI imaging and angiography,
catheter angiography remains the gold standard for diagnosis
of SDAVFs. It also allows for possible endovascular treatment.
SSA reveals tortuous dilated vessels that may span many levels
and a characteristic slow-flow pattern produced by the feeding
dorsal radiculomeningeal artery (Figure 2).
WhilediagnosticSSAis still considered superior toothermo-
dalities for diagnosis, it is not without potential complications.
SSA requires selective catheterization of many spinal feeders
to determine the main feeding artery. This results in lengthy
procedures with extensive exposure to ionizing radiation and
potential nephrotoxic levels of contrast agent.
12
Also, due to
the length of the procedures and the need for complete patient
immobilization,SSAisoftendonewithgeneralanesthesiawhich
presents its own complications.There have also been reports of
neurologic injury caused by catheterization of spinal arteries.
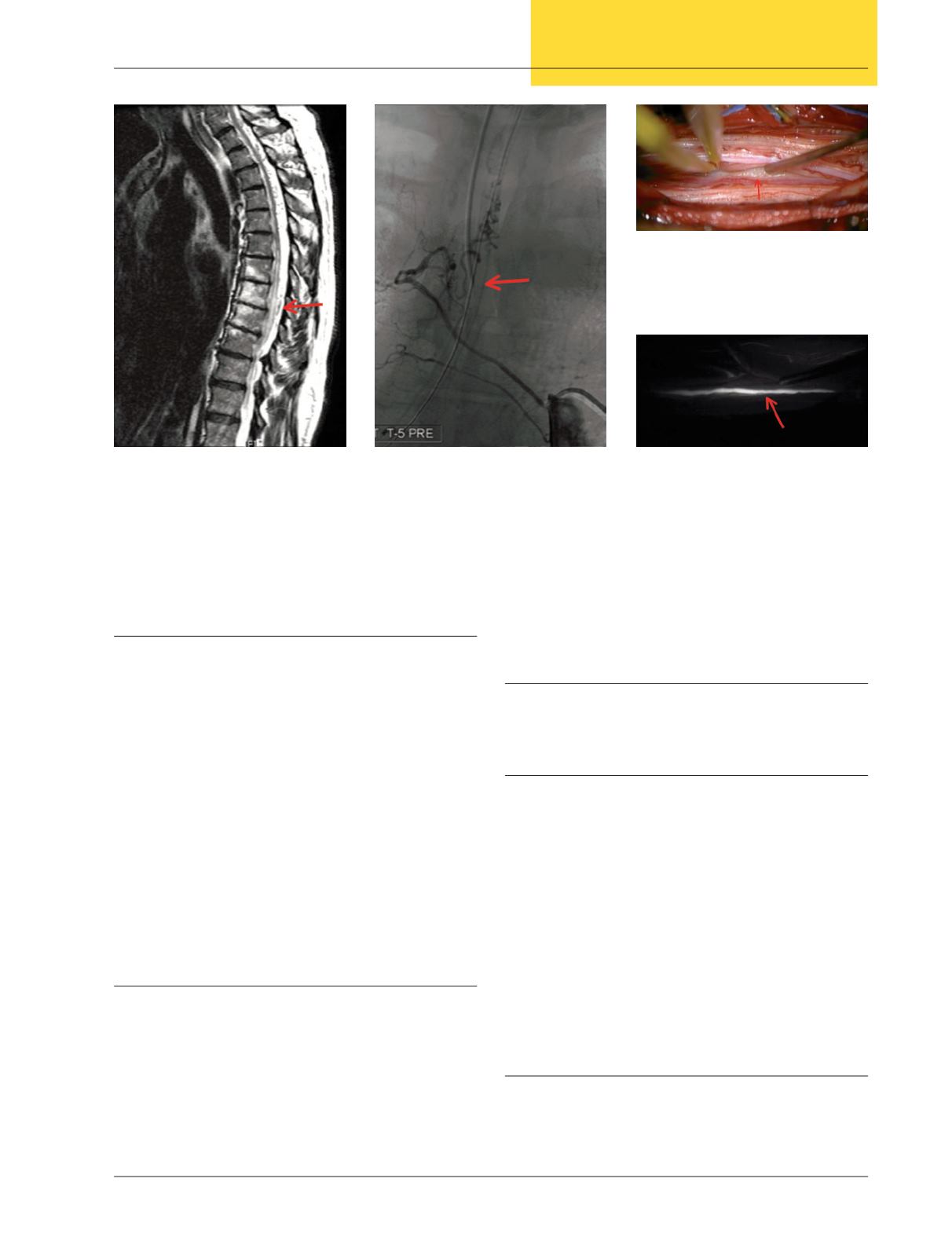
Indocyanine Green Angiography
Indocyaninegreenangiographyhas beenused inophthalmo-
logic procedures to assess the microcirculation of the retina.
14
In the early 2000s, neurosurgeons migrated this technology
to the brain for assistance in clipping cerebral aneurysms.
15
Since this time its use has expanded to the resection of cerebral
arteriovenous malformations, as well as spinal dural arteriove-
nous fistulas. Injection of indocyanine green dye illuminates
the vasculature when viewed with the correct microscope
filter. This allows a surgeon to visualize an early draining vein
and verify that it is no longer filling after ligation of a fistula
(Figures 3a and 3b). This reduces the need for intraoperative
or postoperative selective spinal angiography.
Treatment
Secondary to the progressive nature of this disease,
definitive and prompt treatment is required.
Microsurgical Ligation
Historically, SDAVFswere thought tobeposterior angiomas.
Surgicaltreatmentinvolvedthestrippingofdorsalperimedullary
veins.Thisoftenresulted inworseningofneurologic function. It
was discovered that, instead, treating the intradural arterialized
vein at the nerve root was the appropriate course of action.
Therefore, surgery involves performing a hemilaminectomy,
opening the dura, and following the dorsal radiculomeningeal
artery as it heads towards the dorsal nerve root and ligating the
artery-vein connection by coagulation or clipping. Surgery
has been shown to be associated with very low morbidity (2
percent), with complete occlusion achieved in >98 percent of
cases.
16
Recurrence ratehas beenestimatedat around17percent
via the surgical approach.
17
Endovascular Embolization
The recent advances inendovascular techniqueshaveprovided
an alternative to surgical treatment of SDAVFs. It is less invasive
and may be performed at the same time as the diagnostic an-
Figure 1:
T2 Sagittal MRI showing
tortuous vasculature on the dorsal aspect
of the spinal cord and signal change
within the cord representing edema.
Figure 2:
Spinal angiogram showing
a dorsal intradural SDAVF filling from
the right at T5
Figure 3a:
Intraoperative image of a
ligation of a sacral dural arteriovenous fistula.
The draining vein (arrow) can be seen amidst
the nerve roots of the cauda equina.
Figure 3b:
After injecting indocyanine
green and applying the microscope filter, the
draining vein is clearly visible and fills prior to
the normal vasculature.