34
Vol. 66, No. 3 2015
Northeast Florida Medicine
Endovascular Neurosurgery
Epidemiology
SDAVFs are the most common spinal vascular malforma-
tion. They comprise approximately 70 percent of all spinal
vascular malformations
5
and affect males over females 5:1, as
do cerebral dural arteriovenous fistulas.The annual incidence
is estimated at 5-10/million.
6
These are most frequently di-
agnosed in the 5
th
to 6
th
decades of life.
8
They are located in
the thoracolumbar area in greater than 80 percent of cases,
but can be found in the sacral and cervical regions.
5,7,8
Anatomy
SDAVFs occur when a single radiculomeningeal artery
connects pathologically with a medullary vein. This con-
nection typically occurs in the dural sleeve surrounding the
nerve root within the intervertebral foramen.
9
The radicu-
lomeningeal artery supplies the nerve roots and meninges,
but not necessarily the spinal cord parenchyma. There are
two subtypes: Subtype A involves a single feeding artery,
while Subtype B involves multiple feeders that converge
into a single fistula.
4
The exact etiology of these shunts is
not clear, but venous outflow obstruction is thought to play
a role. SDAVFs are acquired lesions and most likely result
from traumatic injury, infection, or prior surgery; although,
often, the causative agent is never identified.
Pathophysiology
Foix and Alajouanine first described the pathology of
SDAVFs in 192610 as a progressive subacute necrotizing
myelopathy. Their research found evidence of vascular
obstruction, spinal cord necrosis and tortuous and dilated
vasculature on the surface of the spinal cord. This set of
signs and symptoms is now known as Foix-Alajouanine
syndrome. The actual etiology of the noted pathology was
not defined until Aminoff and Logue proposed that it was
venous congestion and venous hypertension that resulted in
cord ischemia.8Venous hypertension results in arterialization
of the coronal venous plexus,
4
which leads to a decreased
pressure gradient between the artery and vein and, therefore,
decreased venous drainage of the spinal cord. This results
in progressive venous congestion and edema of the spinal
cord parenchyma with progressive symptoms.
Clinical Manifestation
Aminoff et al. also characterized the clinical presentation
of their patients with SDAVF.They found that the symptoms
arose gradually and tended to progress.They also noted that
SDAVF led to severe disability in approximately half of the
patients.
8
Early symptoms of SDAVFs are often non-spe-
cific and may lead to delay in diagnosis. These lesions are
often mistaken for more prevalent degenerative disorders
of the spine or even primary neurologic disorders, such
as multiple sclerosis or myelitis. If left untreated, there is
a progressive myelopathy. The most common presenting
symptom is lower extremity weakness, which is seen in about
half of cases
11
; although, in retrospect, patients will report
milder symptoms months to years prior to presentation.
The other symptoms that can be seen at presentation vary
widely. In order of descending frequency these include
gait disturbance, paresthesias, back pain and bladder or
sexual dysfunction.
11
Fortunately, SDAVF rarely presents
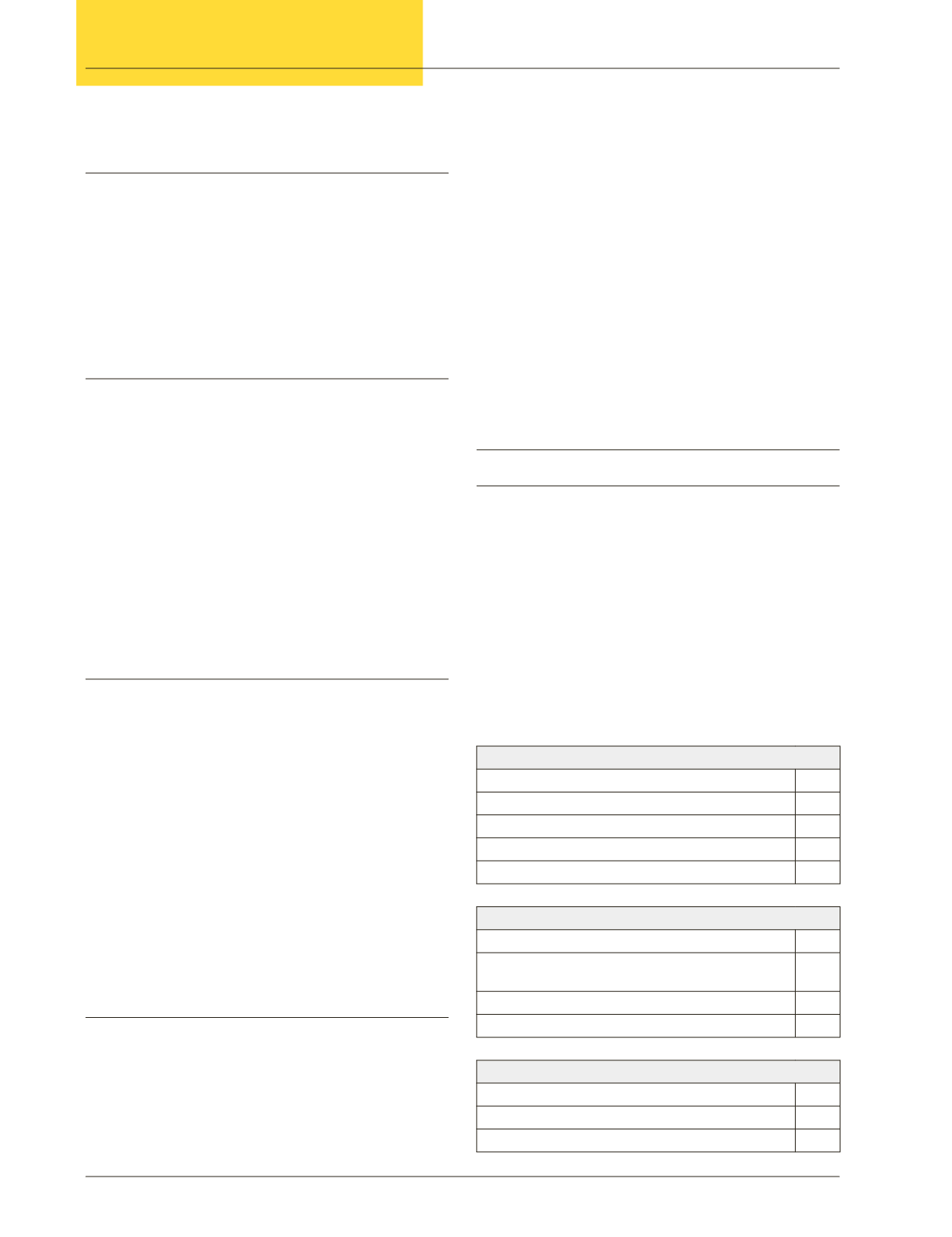
with hemorrhage. Patients are graded clinically based on
the Aminoff-Logue Scale (ALS) (Table 2), which is a useful
tool to follow a patient’s progress over time.
8
Imaging
Magnetic Resonance Imaging
The initial imaging modality to evaluate a suspected
SDAVF should be magnetic resonance imaging (MRI).
Cord edema will manifest itself as increased signal intensity
at the center of the cord on T2-weighted MRI images and
may span several levels. Dorsal intradural flow voids may
be present and are more evident on T2-weighted images
or contrast-enhanced T1-weighted images. Magnetic reso-
nance angiography can sometimes locate the actual fistula
Table 2. Spinal angiogram showing a dorsal
intradural SDAVF filling from the right at T5
Gait
Score
Leg weakness present, but able to walk without assistance
1
Decreased exercise tolerance
2
Requires a cane to ambulate
3
Requires two canes or crutches to ambulate
4
Requires a wheelchair, unable to stand with assistance
5
Micturation
Normal
0
Hesitancy, urgency, frequency, altered sensation,
but remains continent
1
Occasional urinary incontinence or retention
2
Total incontinence or retention
3
Bowel
Mild constipation
1
Intermittent incontinence or persistent constipation
2
Persistent incontinence
3