28
Vol. 66, No. 3 2015
Northeast Florida Medicine
Endovascular Neurosurgery
Unruptured Aneurysms
The large majority of asymptomatic unruptured aneurysms
arediscovered incidentally, onbrainCTorMRI studies ordered
by referring physicians. Symptomatic unruptured aneurysms
may cause symptoms from mass effect and compression of
adjacent neurovascular structures, inflammation related to
aneurysm thrombosis or rapid aneurysm expansion. Symp-
tomatic aneurysms have worse natural history compared to
asymptomatic lesions and thus warrant prompt treatment.
Acutelysymptomaticaneurysmsshouldprompttheworkupfor
SAH, sudden increase in aneurysm size or less frequently, acute
aneurysm thrombosis. The prototypical scenario is a posterior
communicating aneurysm that produces the subacute onset
of a third cranial nerve palsy, warranting accelerated imaging
and treatment.
Asymptomatic aneurysms frequently place the treating
physician in a clinical dilemma, because the benefit of treat-
ment must be superior to the natural history. Also, the benefit
of intervening upon asymptomatic lesions is not nearly as
demonstrable as it is in symptomatic or ruptured aneurysms.
Management decisions are rarely straightforward.
There are currently no strict guidelines. The decision
making process is based on unbiased assessment of patient
history and lesion characteristics, and available data regarding
all treatment modalities. Observational cohort studies of
unruptured aneurysms have identified several factors that can
alter the rate of aneurysm formation and rupture.
4-8
These
include: family history of SAH, cigarette smoking, presence of
symptoms attributable to the lesion, irregular shape, narrow
aneurysm neck, size relationship between aneurysm/parent
vessel, aneurysm location, and most prominently, aneurysm
size 4-8 (Tables 1 and 2). Aneurysm size is the single strongest
predictor of aneurysm rupture, yet it should never be used as
the sole indicator. Generally, a 7 mm aneurysm diameter is the
best cut-off point for an increased risk of hemorrhage (Table
3). ISAT investigators found that the mean size of ruptured
lesions was around 5 mm, showing a potential role for treating
smaller unruptured lesions1. Aneurysm location is also an
important factor to consider. For example, lesions located in
the posterior circulation (vertebral artery, basilar artery, and
posterior inferior cerebellar artery), posterior communicating
artery and, more recently, anterior communicating artery have
increased risk of rupture.4,8 In contrast, aneurysms located in
the cavernous segment of the internal carotid artery havemuch
lower riskof ruptureunless symptomaticor larger than13mm.8
Exercise cautionwhendealingwith so-called cavernous lesions.
Transition aneurysms (lesions past the “distal dural ring” and
located in the subarachnoid space) may be mistakenly labeled
as cavernous aneurysms.Transitionaneurysms behave clinically
as non-cavernous lesions and must be dealt with as such.
Cigarettesmokinghasbeenassociatedwithahigherlikelihood
of developing intracranial aneurysms, accelerated aneurysm
growth and increased risk of rupture.
4,9
First-degree relatives
of patients with aneurysms also have an increased risk of
harboring an incidental lesion. Individuals with one first-de-
gree relative affected have an increased risk of 4 percent
to 5.6 percent compared to the general population. That
risk doubles to approximately 8 percent if two first-degree
relatives are affected.
8
Therefore, screening for incidental
lesions is recommended in these circumstances, especially
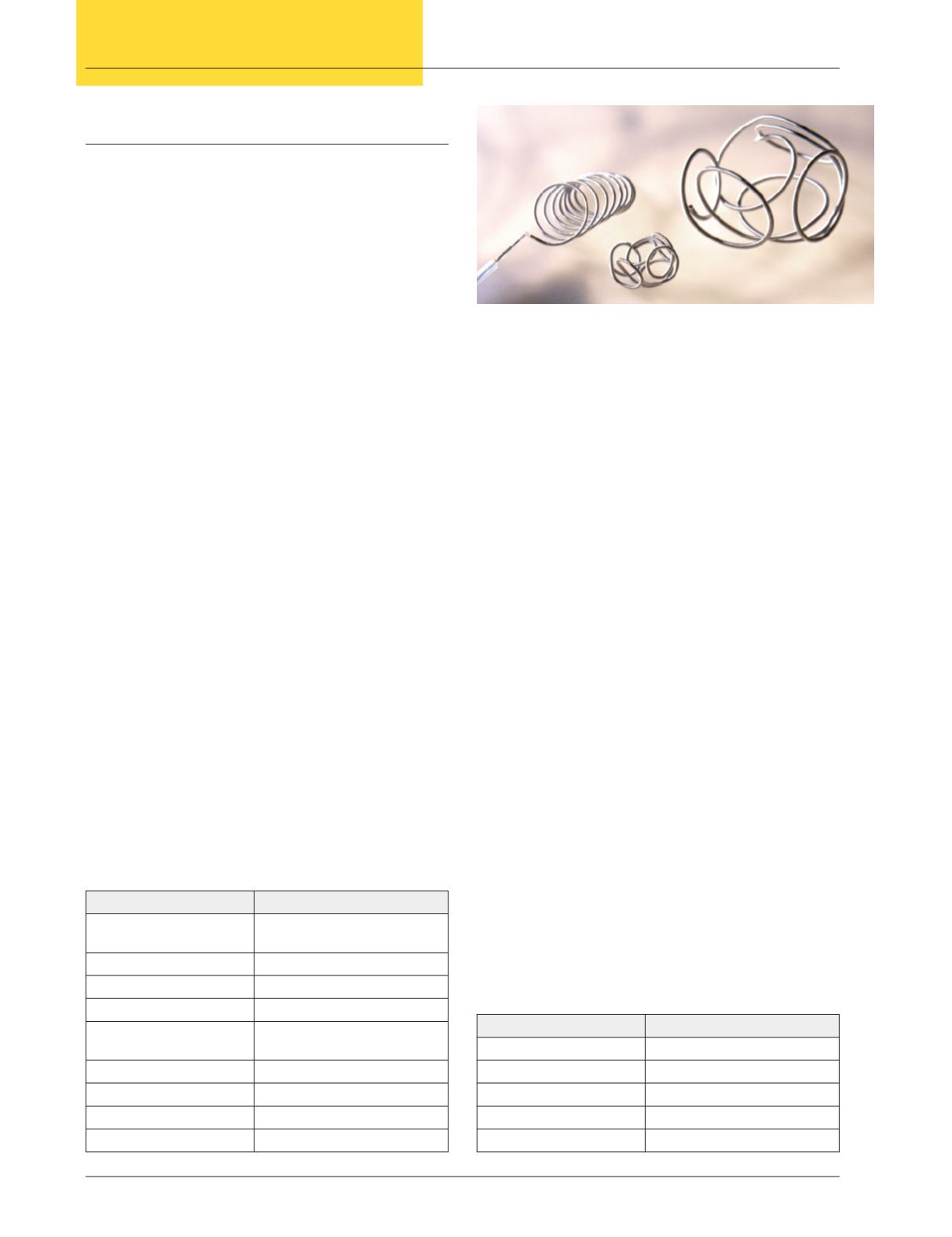
Figure 2:
Detachable embolization coils are used to fill the
aneurysm sac and create stagnation of blood flow, leading to aneurysm
occlusion. Today, these coils are developed to produce 3-dimensional
shapes before being detached inside the aneurysm sac to optimize
filling of the lesion and improve the rates of aneurysm occlusion.
Table 1.
Risk Factors to Develop Intracranial Aneurysms
General risk factors
Inherited risk factors
Female gender
Autosomal dominant polycystic
kidney disease
Cigarette smoking
Fibromuscular dysplasia
Hypertension
Type IV Ehlers-Danlos syndrome
Age over 50 years
Alpha1-antitrypsin deficiency
First-degree relative with
aneurysm
Hereditary hemorrhagic telangi-
ectasia
Cocaine use
Pseudoxanthoma elasticum
Infection of vessel wall
Neurofibromatosis type 1
Neoplastic emboli
Pheochromocytoma
-
Tuberous sclerosis
Table 2.
Risk Factors for Aneurysm Rupture
Patient-related
Aneurysm-related
Cigarette smoking
Aneurysm size
Previous SAH
Aneurysm location
-
Irregular shape (daughter sac)
-
Narrow neck
-
Parent vessel/aneurysm relation