24
Vol. 66, No. 3 2015
Northeast Florida Medicine
Endovascular Neurosurgery
the cortex involved (Table 1).
9
Large (> 6 cm) lesions, deep
venous drainage, and eloquent cortex have been associated
with worse surgical outcomes (Table 2).
Radiosurgery
Radiosurgery has emerged as a safe method for the treat-
ment of small AVMs.
10,11
Radiosurgery involves the use of
stereotactic localization to precisely focus a large dose of
radiation onto a lesion, and is oftentimes performed in a
single treatment. This treatment modality is particularly
attractive for small, deep-seated AVMs. AVMs with vol-
umes equal to or less than 10 ml have a 78 to 88 percent
obliteration rate at three years.
12
The disadvantage of this
form of treatment is the risk of hemorrhage during the 2-
to 3-year lag time until AVM obliteration occurs.
Endovascular Therapy
The endovascular treatment strategy for an AVM is
significantly influenced by the overall treatment plan for
any given AVM and any given patient. Endovascular AVM
embolization strategies can be considered within the fol-
lowing categories of goals and issues: (1) embolization as
a presurgical tool, (2) embolization as a pre-radiosurgery
tool, (3) embolization alone as a curative modality, (4)
embolization for palliation of symptoms, and (5) emboli-
zation of associated aneurysms.
Embolization reduces the amount of blood loss that is
associated with AVMresection by decreasing the vascularity
of the nidus.
13
Embolized AVM vessels can also serve as a
roadmap during surgery by helping the surgeon define the
anatomy of the feeding pedicles and the nidus. Despite
these advantages, AVM embolization carries considerable
risk. In presurgical planning of AVM embolization, a
physician must embolize those pedicles felt to be the most
technically challenging to access during surgery (Figure 2).
For the radiosurgery patient, embolization strategies
have been used to reduce the volume of an AVM and to
eliminate the pedicle and proximal aneurysms. The size of
an AVM nidus influences the success of radiosurgery.10
Hence, reducing the size of an AVM with embolization
may increase the success rate of radiosurgery and help avoid
using the higher radiation doses needed to treat a larger
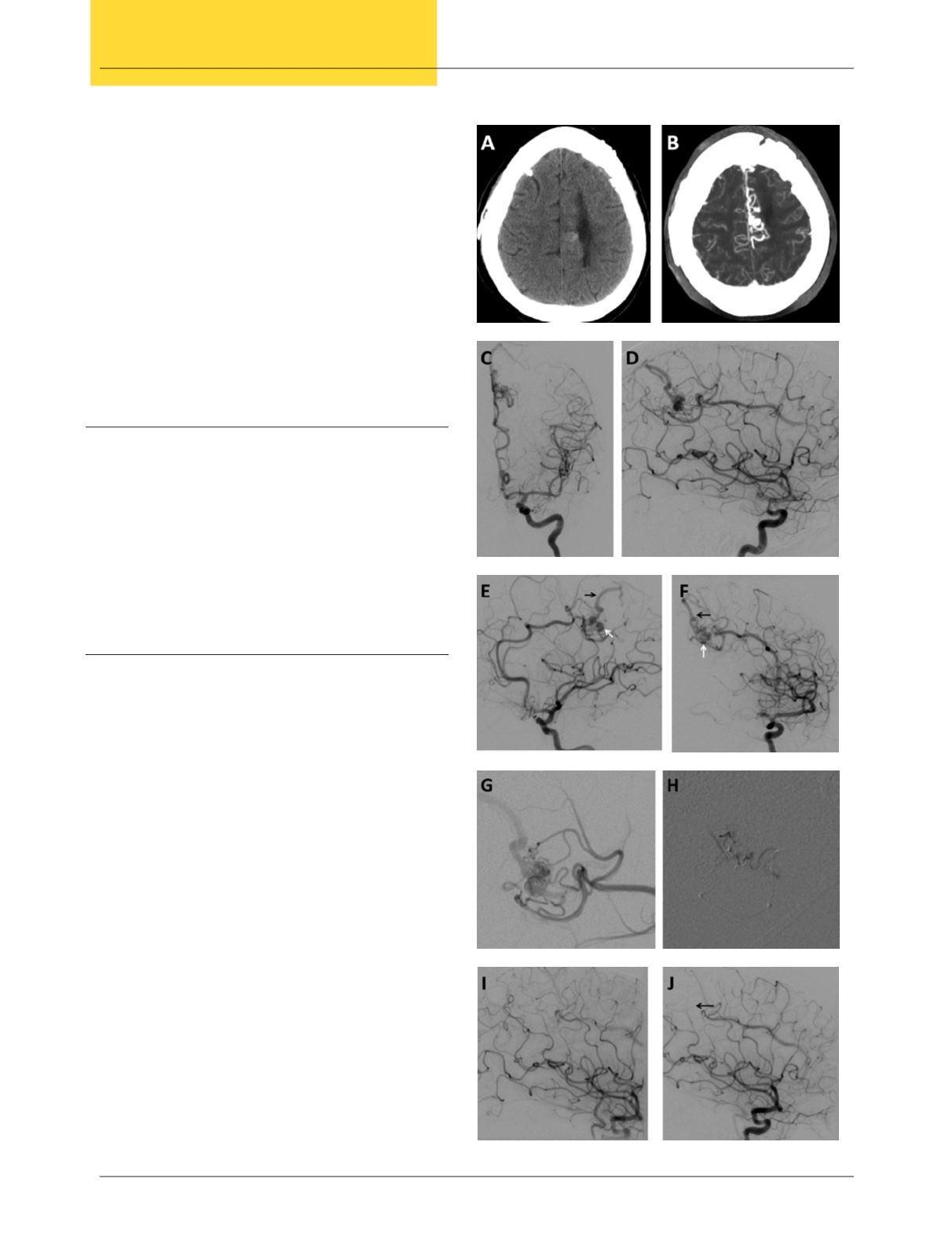
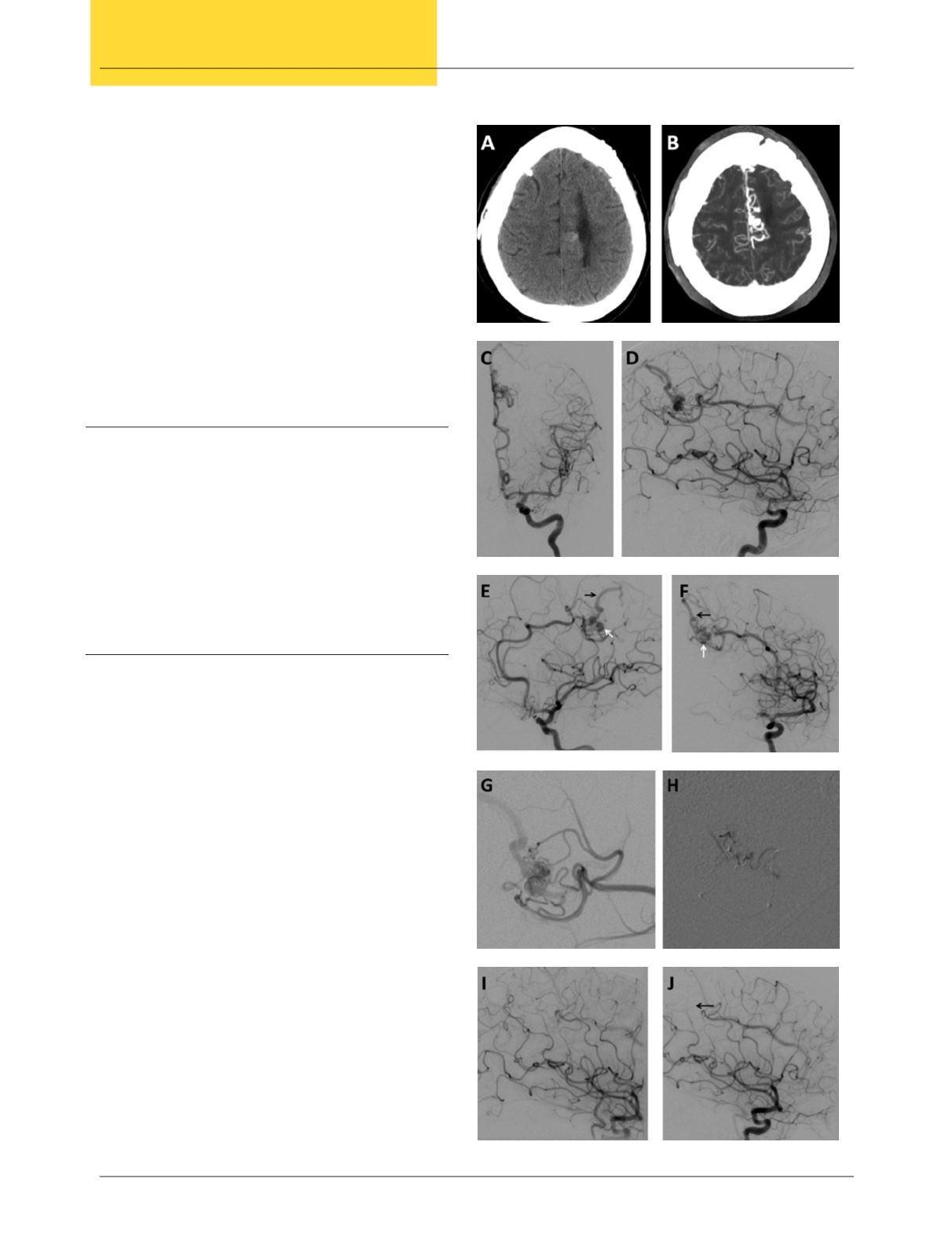
Figure 3.
A 40-year-old female was diagnosed with a left
AVM. (A) CT scan and (B) and post-contrast MRI showed
a small AVM located near the midline in the frontoparietal
region. (C-F) DSA in multiple views demonstrated the AVM
nidus (white arrows) and superficial draining veins (black
arrows). (G) Selective contrast injection depicting in detail the
arterial feeders and venous drainage of the AVM as well as (H)
post-embolization results. (I-J) DSA after complete occlusion
of the AVM with embolization agent (black arrow).