22
Vol. 66, No. 3 2015
Northeast Florida Medicine
Endovascular Neurosurgery
Arteriovenous Malformations: A Review of Epidemiology,
Pathology, and Management Options in the Modern Era
By Ramesh Grandhi, MD, Richard Williamson, MD, Leonardo B. C. Brasiliense, MD,
Eric Sauvageau, MD, Ricardo A. Hanel, MD, PhD
Lyerly Neurosurgery, Baptist Health, Jacksonville, FL
Introduction
An arteriovenous malformation (AVM) is a collection of
abnormal veins and arteries that lack a normal intervening
capillary bed. The lack of the capillary bed creates a low-re-
sistance system and results in high-velocity blood flow
(arteriovenous shunting) and venous hypertension. High
flow results in vascular recruitment and arterialization of
venous structures.
2,3
An AVM can be divided structurally
into three components: arterial pedicle(s) (feeding vessels),
nidus, and draining vein(s). The nidus is a conglomeration
of densely packed abnormal vessels with minimal or no
intervening tissue. It is believed that AVMs are most often
Address correspondence to:
Ricardo A. Hanel, MD, PHD
800 Prudential Drive – Suite #1100
Jacksonville, FL 32207
Telephone: 904-388-6518
Fax: 904-384-1005
Email:
Abstract:
Intracranial arteriovenous malformations (AVMs)
represent an uncommon vascular pathology with a yearly hemorrhage
rate of upwards of four percent.
1
Defined as a collection of veins and
arteries without an intervening capillary bed, AVMs are congenitally
acquired lesions that are often asymptomatic; when symptomatic,
patients may experience headaches, seizures or ischemic symptoms.
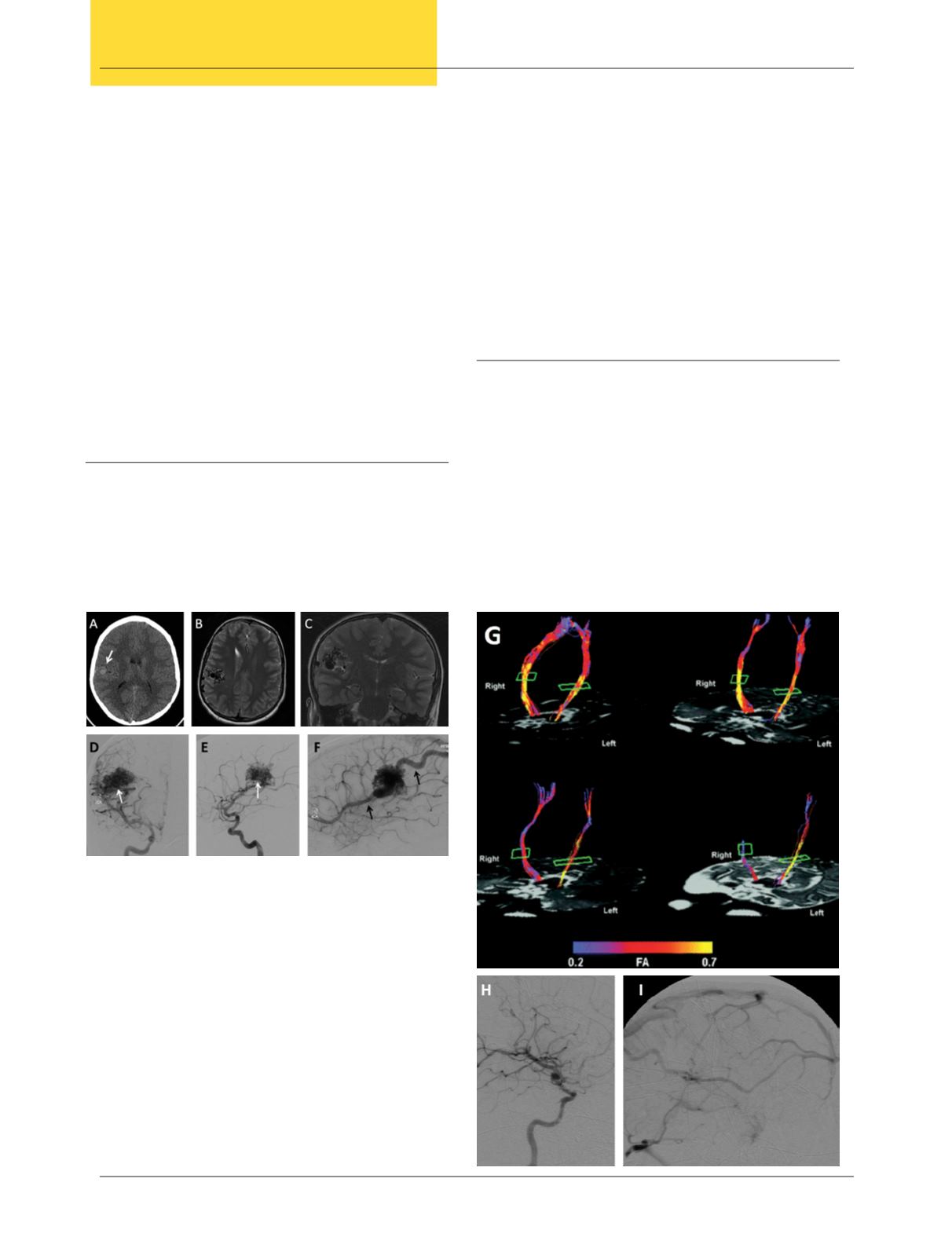
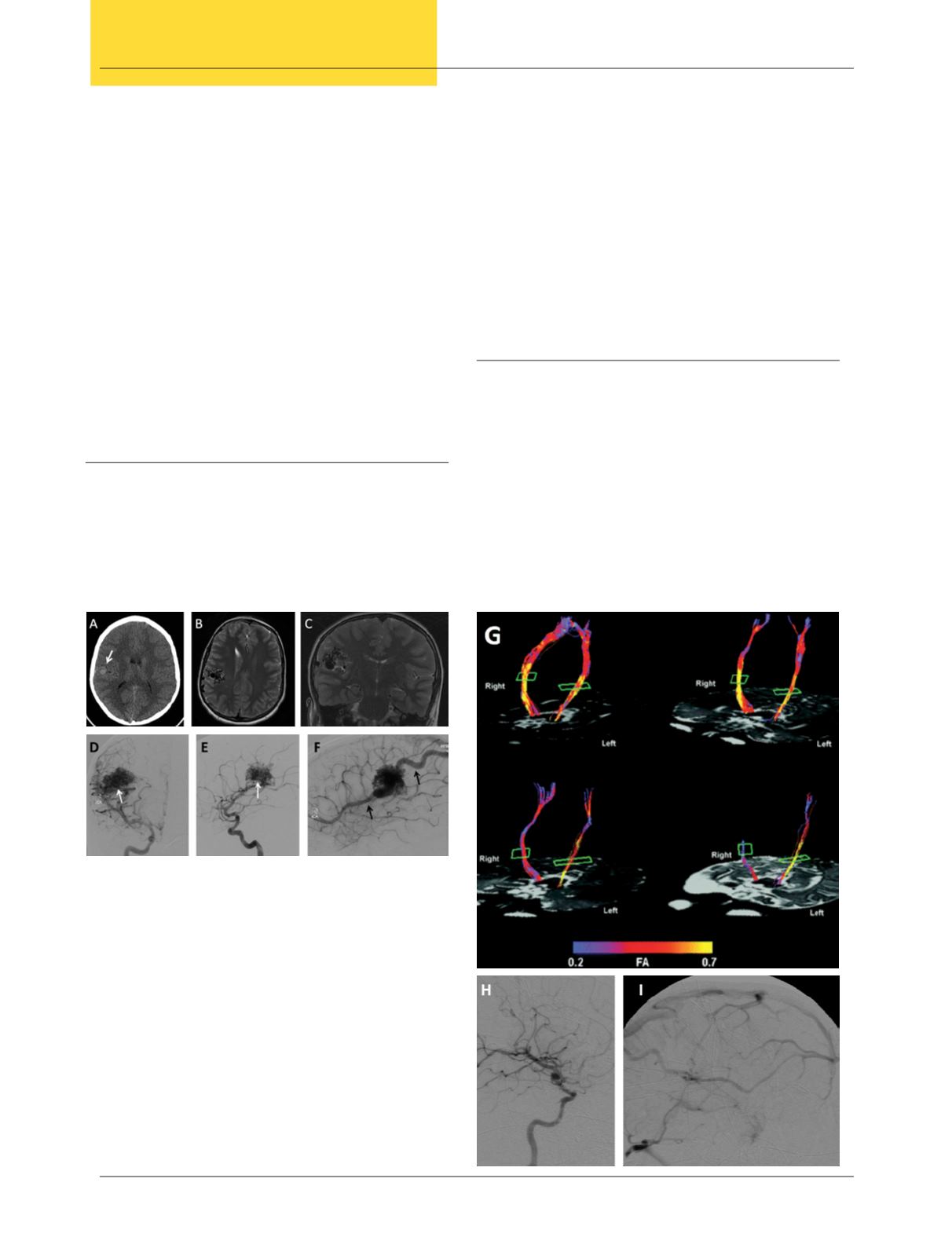
Figure 1.
A 14-year-old male with seizures was referred
to our institution. (A) Computed tomography (CT) scan
demonstrated a heterogeneous hyperdense lesion on the right
parietal lobe (white arrow). (B) Magnetic resonance imaging
(MRI) revealed an AVM located in the parietal lobe and (C)
extending into the sylvian fissure. (D-F) Digital subtracted
angiograpy (DSA) in multiple views showed the AVM nidus
(white arrows) and venous drainage (black arrows). For surgical
planning, we obtained (G) tractography and mapping of motor
area, which provides more detailed information regarding the
location of motor fibers and their relationship to the AVM.
A stealth-guided craniotomy was performed and complete
resection of the lesion was achieved. (H-I) Follow-up DSA
demonstrated no residual contrast filling of the AVM.